How do moisture and temperature impact pressure injury risk?
Pressure injury risk assessment and prevention are important aspects in caring for patients, impacting 1 in 10 hospitalized patients1 and often leading to extended hospital stays, surgery, and infection.2 Specifically for patients in the ICU requiring prone positioning, the incidence of pressure injury is significant, ranging from 25-48%.3
Pressure injury prevention requires an understanding of the underlying factors causing pressure injury. These include friction, shearing, moisture, temperature, nutrition, comorbidities, and limited mobility.2 While some of these factors require medical interventions, others can be reduced by implementing products designed to reduce aspects such as friction, shearing, moisture, and temperature.
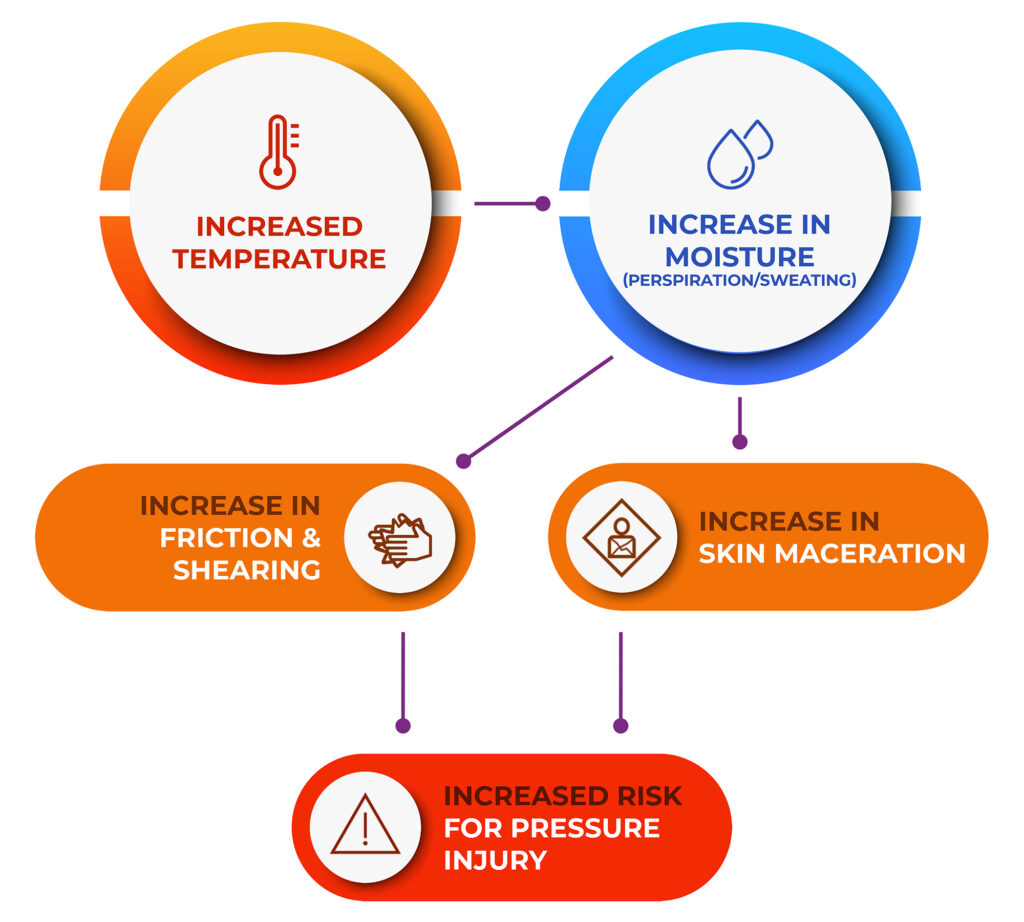
Moisture and temperature are significant in pressure injury prevention. Immobile, hospitalized patients are at increased risk for temperature elevation due to being in contact with a surface for an extended period. This causes insulated, trapped heat at the skin surface. Prevention of this insulation and its resulting increase in temperature is important to regulate, since we know that increases in temperature can lead to perspiration, ultimately causing moisture accumulation.4,5 When moisture accumulates, skin integrity is compromised and vulnerable due to increases in skin maceration, friction and shearing, increased skin susceptibility to tearing and abrasions, and reduction in nutrient supply.6-16 To summarize, reducing temperature and moisture at the skin surface is critical to protect against pressure injury.
While there are several products available for skin temperature and moisture management, these products focus on reducing pressure injury risk for patients in the supine position. For the prone position, there are few viable choices available to clinicians providing pressure redistribution with moisture and temperature reduction.
The InteliDerm™ Powered Skin Protection System is part of the Pronova-O2™ Automated Prone Therapy System and provides the added benefit of pressure injury prevention with moisture and temperature management for the face and chest! The Pronova-O2 Automated Prone Therapy System provides a safe and efficient method for positioning critically ill patients. INQUIRE NOW to request a demo for your facility! For additional information on automated prone positioning, please visit turnmedical.com or call 1-855-275-8876.
Refer to Pronova-O2 Instructions for Use for full prescribing information including risks.
References
- Bluestein, D. and Javaheri, A. (2008). Pressure Ulcers: Prevention, Evaluation, and Management. American Family Physician, 78(10), pp. 1186–1194. Retrieved February 14, 2022 from https://www.aafp.org/afp/2008/1115/afp20081115p1186.pdf.
- Li, Z., Lin, F., Thalib, L., and Chaboyer, W. Global prevalence and incidence of pressure injuries in hospitalised adult patients: A systematic review and meta-analysis. Int J Nurs Stud. 2020 May;105:103546. doi: 10.1016/j.ijnurstu.2020.103546. Epub 2020 Jan 31. PMID: 32113142.
- Patton, D. et al. (2021). The effect of prone positioning on pressure injury incidence in adult intensive care unit patients: A meta-review of systematic reviews, Australian Critical Care, ISSN 1036-7314, https://doi.org/10.1016/j.aucc.2021.10.003.
- Bullard, R. W., Banerjee, M. R., Chen, F., Elizond, R., and MacIntyre, B. A. (1970). Skin Temperature and Thermoregulatory Sweating: A Control Systems Approach. In Physiological and Behavioral Temperature Regulation, Hardy, J. D., Gagge, A. P., Stolwijk, J. A., Eds., Chapter 40: 597–610.
- Nadel, E. R., Bullard, R. W., and Stolwijk, J. A., Importance of Skin Temperature in the Regulation of Sweating. Appl. Physiol. 1973:31(1), 80–87.
- Brandis, K. (2008). Fluid Physiology: An Online Text. http://www.anaesthesiaMCQ.com
- Leyden, J. J. (1984). Corn Starch, Candida Albicans, and Diaper Rash. Pediatric Dermatology (4): 322–325.
- Leyden, J. J., Katz, S., Stewart, R., Kligman, A. M. (1977). Urinary Ammonia and Ammonia-Producing Micro-Organisms in Infants with and without Diaper Dermatitis. Archives of Dermatology 113(12): 1678–1680.
- Zimmerer, R. E., Lawson, K. E., and Calvert, C. J. (1986). The Effects of Wearing Diapers on Skin. Pediatric Dermatology. 3(2): 95–101.
- Schell, V. C. and Wolcott, L. E. (1976). Etiology, Prevention, and Management of Decubitus Ulcers. Med. 63: 109–112.
- Flam, E. Skin maintenance in the bed-ridden patient. Ostomy/Wound Management 1990; 28: 49–54.
- Park, A. and Baddiel, C. Rheology of stratum corneum-I. Journal of the Society of Cosmetic Chemists 1972; 23: 3–12
- Wildnauer, R., Miller, D., and Humphries, W. A physicochemical approach to the characterization of stratum corneum. R. Baier, Ed., Applied Chemistry at Protein Interfaces, Advances in Chemistry Series (American Chemical Society) 1975, vol. 145 (Chapter 4).
- Kokate, J. Y., Leland, K. J., Held, A. M., Hansen, G. L., Kveen, G. I., Johnson, B. A., et al. Temperature-Modulated Pressure Ulcers: A Porcine Model. Phys Med Rehabil. 1995:76:666–673.
- Patel, S., Knapp, C. F., Donofrio, J. C., Salcido, R. Temperature Effects on Surface Pressure-Induced Changes in Rat Skin Perfusion: Implications in Pressure Ulcer Development. Journal of Rehabilitation Research and Development. Vol 36 No. 3 July 1999
- Ruch, R. C. and Patton, H. D., eds. (1965) Physiology and Biophysics, 19th ed. Philadelphia, Pa.: WB Saunders. 1030–1049.






